(BPT) - Sponsored by Intercept Pharmaceuticals
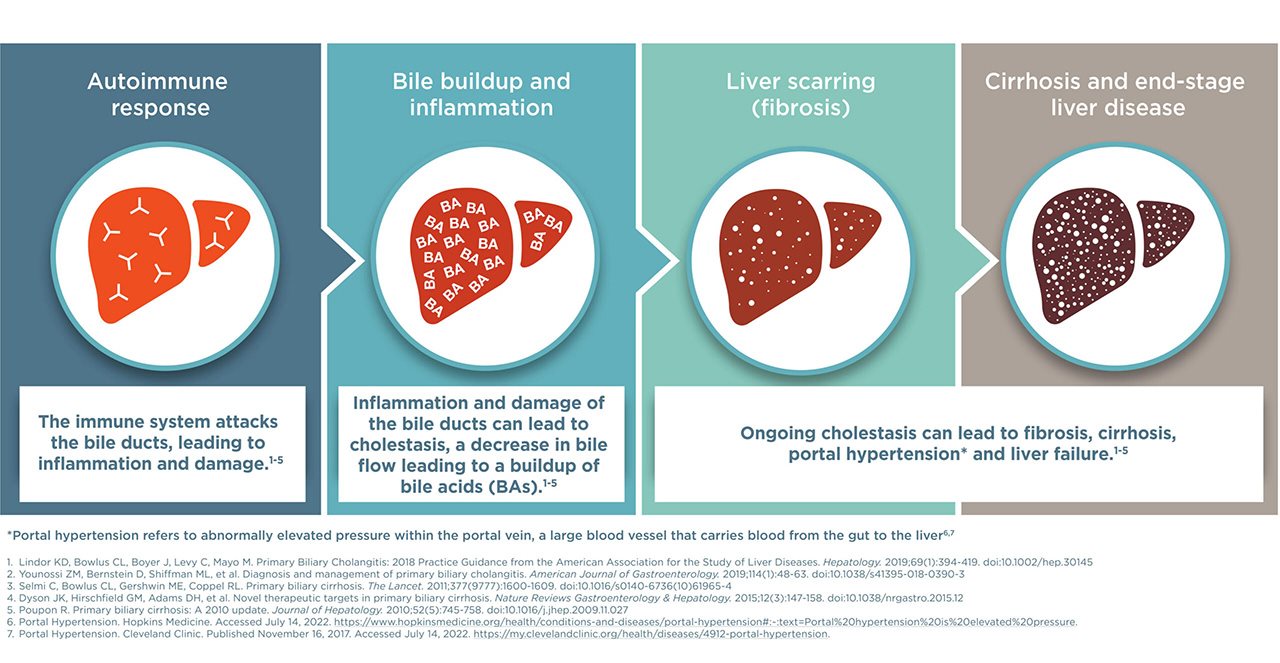
Primary biliary cholangitis (PBC) is a rare liver disease that causes the body to attack its own cells in the bile ducts of the liver. Bile ducts are tube-like structures that carry bile from the liver to the intestine to help digest food. However, when bile can't flow through the bile ducts, it collects in the liver and causes damage.
The most common early symptoms of PBC are pruritis (itching) and fatigue, though some PBC patients do not show symptoms at the time of diagnosis. If PBC progresses, it can cause an increase in risk of liver cancer, the need for liver transplant and death.
There is no cure for PBC, however, there are treatment options that can help people manage their disease. In recognition of September's PBC Awareness Month, let's look at five key facts about this condition and hear from healthcare providers, advocates and people living with PBC:
Fact #1: PBC is progressive and chronic, which means it won't just go away and can get worse over time
Damage from PBC can cause fibrosis (scarring) and, in its most severe form, lead to cirrhosis (severe scarring). In some cases, this can result in liver failure and the need for a liver transplant.
Dr. Kris Kowdley, Director of the Liver Institute Northwest and Professor of Medicine at Elson S. Floyd College of Medicine at Washington State University, explained, 'PBC can progress slowly for some people, while others may advance to end-stage liver disease or liver failure much more rapidly. Therefore, it's important to catch it as early as possible so that we can treat the disease to slow the rate of progression and minimize the amount of damage and scarring to the liver. With early detection, we can hopefully reduce the risk of the patient developing cirrhosis or other complications of liver disease.'
Fact #2: Because many people with PBC have no symptoms, the disease is often discovered from abnormal results on routine liver blood tests
Most people with PBC do not experience symptoms at the time of their diagnosis. Instead, it is detected during routine blood tests which assess damage to the liver by measuring different enzymes and proteins in the blood.
One of the key enzymes used to help diagnose PBC is alkaline phosphatase, or ALP, which can also monitor disease progression and track how well someone is responding to treatment. More recent studies have shown that other liver enzymes beyond ALP are also important in assessing total liver health. Treatment can help improve these enzymes and reduce liver damage.
Dr. Kim Brown, Division Chief of Gastroenterology and Hepatology and the Associate Medical Director of the Henry Ford Hospital Transplant Institute, stated, 'We typically look at ALP levels when assessing PBC, though recent research shows that there are several biomarkers that should be measured and assessed. While still considered the cornerstone of PBC evaluations, we now look beyond ALP to include other liver enzymes as well as liver fibrosis when evaluating total liver health.'

Fact #3: While PBC is more common in females, it can affect anyone
People with PBC have historically been portrayed as middle-aged Caucasian women; however, it is widely recognized now that men and people of color are affected in higher numbers than once believed.
Wayne, a man living with PBC, was diagnosed in 1992, and before his diagnosis, the only person he knew with PBC was his father. He was shocked when he walked into his first PBC support group meeting and was surrounded by women. While more common in females, PBC can impact individuals from any background and may also be hereditary. A PBC diagnosis is often delayed among males because of the myth that PBC is rare in males, thus, the disease course in males tends to be more aggressive with worse outcomes.
Research also suggests that people of color living with PBC tend to have more severe disease when first diagnosed and experience worse long-term outcomes.
As Donna Cryer, a key advocacy leader and Founder, President and CEO of the Global Liver Institute, stated, 'No matter who you are, you should be able to receive timely and thorough diagnosis and care for PBC. Equitable care for PBC patients requires us to move beyond harmful stereotypes and improve the system so that everyone has the same opportunity.'

Fact #4: PBC was once called primary biliary cirrhosis
For many years, PBC wasn't diagnosed until it was late-stage and patients had already developed cirrhosis. Unfortunately, the negative stigma associated with cirrhosis led some people to incorrectly believe PBC was related to alcohol consumption.
Almost 10 years ago, a dedicated group of patient leaders and medical professionals, with the support of industry partners including Intercept Pharmaceuticals, teamed up and advocated to have the name changed to more accurately reflect the disease. Carol Roberts, President of the PBCers Organization who played a pivotal role in the movement, said, 'Prior to the name change many patients did not share their diagnosis with others, even friends and family, because of the stigma. This prevented them from receiving the support they needed while dealing with the diagnosis. The name change helps them feel more comfortable sharing the diagnosis, allowing them to receive support and understanding, while increasing awareness of PBC.'

Fact #5: Even with initial treatment, up to 50% of people have uncontrolled disease
For many people, the first treatment their doctor prescribes is not enough to adequately control their PBC. Medical guidelines recommend that liver function tests are repeated every three to six months to monitor the disease and help determine if their initial treatment is working, or if additional therapy should be considered.
With this, it's important for people with PBC to talk to their doctor about symptoms and test results to understand how they're responding to treatment and if more can be done.
Visit LivingwithPBC.com for helpful resources, including discussion guides, tips for managing symptoms, patient videos and the PBC Living® app that tracks test results.